Autor :Aren, Leandro1, Mayer, Germán F. 1, Hernández, Julián1
1 Kinesiology Service, Intensive Care Unit. Hospital Madre Catalina RodrĂguez. Merlo, San Luis. 2Intensive Care Unit. Hospital Madre Catalina RodrĂguez. Merlo, San Luis.
https://doi.org/10.56538/ramr.NPEQ9628
Correspondencia : Leandro Aren. E-mail: leann.mdp@gmail.com
ABSTRACT
Heterotopic ossification (OH) is defined as the formation of bone tissue
in areas of soft tissue where there is usually no bone. It is a
rare/underdiagnosed pathology usually related to paralysis and immobilization
during the critical course of trauma, neurological lesions, acute respiratory
distress syndrome (ARDS), surgery, or major burns. In the course of the
SARS-CoV2 (new COVID-19) pandemic, cases of critically ill patients with OH
were reported, interpreting that the magnitude of the inflammatory reaction,
possible effect of the virus itself, and long periods of immobilization while
the critical stage was taking place could be the determinants of this clinical
entity.
During the hospitalization period of the cases that we will describe
below, the occupational percentage was 166 % and 200 % and the workload of the
nursing staff, measured by TISS-28, was 72 points, exceeding almost twice the
possibilities labor. At the same time, motor rehabilitation by the
Physiotherapy team was postponed due to the need to address urgent
circumstances such as optimization of ventilatory
support and participation in decubitus change maneuvers. In this way, we
interpret that the great work overload that occurred during the pandemic
conditioned an inadequate provision of early mobilization, resulting in a
higher prevalence of OH in severe post-COVID patients when compared with ARDS
due to other causes.
We present two cases of HO in patients who underwent ARDS due to
SARS-CoV2 at times of high workload.
Case 1: A 48-year-old man, who was admitted to the ICU due to severe
Pneumonia (NAC) due to COVID-19. History of obesity.
He required 31 days of Mechanical Ventilation Assistance (AVM), 4 cycles of
prone position (192 total hours), tracheostomy (TQT) on day 18, 23 days of
neuromuscular blockers and 24 of sedation. Active-assisted mobilization begins
on day 24 with a Medical Research Council (MRC) score of 38/60. A total of 52 days of hospitalization. Six months after
discharge, bilateral HO of the hip was diagnosed.
Case 2: 58-year-old patient, admitted to the ICU with severe NAC due to
COVID-19. History of Hypertension and Obesity. She
required 39 days of AVM, two cycles of prone position (60 total hours), TQT on
day 7. A total of 45 days in the ICU and 111 in the hospital.
A year after discharge, bilateral OH of the hip was diagnosed.
Key words: COVID-19, Ossification, Heterotopic
RESUMEN
Se define como osificaciĂłn heterotĂłpica a la
formaciĂłn de tejido Ăłseo en zonas de tejido blando en donde habitualmente no
hay hueso. Se trata de una patologĂa rara/ subdiagnosticada
habitualmente relacionada con parálisis e inmovilización durante el curso
crĂtico de traumatismos, lesiones neurolĂłgicas, sĂndrome de dificultad
respiratoria aguda, cirugĂas o grandes quemados. En el transcurso de la
pandemia por SARS-CoV-2 (nuevo COVID-19), se reportaron casos de pacientes
crĂticos con osificaciĂłn heterotĂłpica y se interpretĂł
que la magnitud de la reacciĂłn inflamatoria, posible efecto propio del virus, y
los largos perĂodos de inmovilizaciĂłn mientras transcurrĂa la etapa crĂtica
podrĂan ser los determinantes de esta entidad clĂnica.
Durante el perĂodo de internaciĂłn de los casos que describiremos a
continuaciĂłn, el porcentaje ocupacional fue del 166 % y del 200 % y la carga
laboral del personal de enfermerĂa, medida por TISS-28, fue de 72 puntos, lo
que excediĂł casi al doble de las posibilidades laborales. Al mismo tiempo, la
rehabilitaciĂłn motora, por parte del equipo de kinesiologĂa, se vio postergada
ante la necesidad de atender circunstancias urgentes como la optimizaciĂłn del
soporte ventilatorio y la participaciĂłn en maniobras de cambios de decĂşbito. De
este modo, interpretamos que la gran sobrecarga laboral acontecida durante la
pandemia condicionĂł una inadecuada provisiĂłn de movilizaciĂłn temprana que dio
como resultado una mayor prevalencia de osificaciĂłn heterotĂłpica
en pacientes pos-COVID grave cuando se la compara con sĂndrome de dificultad
respiratoria aguda por otras causas.
Presentamos dos casos de osificaciĂłn heterotĂłpica
en pacientes que cursaron sĂndrome de dificultad respiratoria aguda por
SARS-CoV-2 en momentos de alta carga laboral.
Caso 1: Paciente masculino de 48 años, que ingresó a la UCI por NAC
grave por COVID-19. Antecedentes de obesidad. RequiriĂł 31 dĂas de AVM, 4 ciclos
de posiciĂłn prona (192 h total), TQT al dĂa 18, 23 dĂas de bloqueantes neuromusculares
y 24 de sedaciĂłn. Comienza la movilizaciĂłn activa-asistida al dĂa 24 con MRC
38/60. Un total de 52 dĂas de internaciĂłn. A los 6 meses del alta, se
diagnosticĂł osificaciĂłn heterotĂłpica bilateral de
cadera.
Caso 2: Paciente de 58 años, que ingresa a UCI por NAC grave por
COVID-19. Antecedentes de HTA y obesidad. RequiriĂł 39 dĂas de AVM, dos ciclos
de posiciĂłn prona (60 h total), TQT al dĂa 7. Un total de 45 dĂas de UCI y 111
de hospital. Al año del alta, se diagnostica osificación heterotópica
bilateral de cadera.
Palabras clave: COVID-19, OsificaciĂłn HeterĂłpica
Received: 02/01/2023
Accepted : 07/25/2023
INTRODUCTION
The SARS-CoV
2 pandemic challenged the majorÂity of the healthcare systems worldwide, with a
high utilization rate of critical care and not enough qualified human
resources. This situation generÂated the need to meet the demand by employing
personnel without the necessary expertise or by increasing the workload of the
staff in those areas. In this context, new publications emerge daily on the
stress experienced by the healthcare system and personnel.1
Patients who suffered from severe
COVID-19 experienced prolonged stays in the ICU, prolonged use of analgosedative and neuromuscular blocking agents, the need
for mechanical ventilatory assisÂtance (MVA), and
extended prone positioning cycles. The simultaneous large number of critical
patients exceeded the capacity of the personnel to provide adequate care, and
this caused potential complicaÂtions related to the stress of healthcare
workers.1,2
Heterotopic ossification (HO)
consists in the formation of bone tissue in areas of extraskeletal
soft tissue where there is usually no bone.3
There are two typical
presentations of HO: heÂreditary and acquired. The latter is more prevalent and
is primarily observed in patients with proÂlonged immobilization following
musculoskeletal traumatic injuries, neurological injuries, major burns, ARDS,
or major surgeries.4
Prolonged immobilization is a
common factor among patients with traumatic brain injury, spinal cord injury,
ARDS from other causes, and severe COVID-19.5
Tissue injury results in the
invasion of inflamÂmatory cells, causing an alteration in cells with mesenchymal origin. This impairment can lead to an osteogenic or osteochondrogenic
program as mesenchymal cells differentiate into
osteoblasts.6 The systemic inflammation, altered calcium meÂtabolism, and
local myositis seen in patients with COVID-19 could potentially trigger this
effect.7
Recently, HO has been reported as
a complicaÂtion associated with severe COVID-19 patients who underwent extended
periods of MVA and prolonged hospital stay.7
In the vast majority of cases,
heterotopic ossification was identified after hospital discharge, with pain,
limited range of motion, and joint stiffness as the symptoms that triggered
suspicion. Subsequently, the diagnosis was confirmed through imaging studies.5,8,9
CASE REPORT 1
A 43-year-old male patient was
admitted to the ICU for severe COVID-19 pneumonia, after two days of
hospitalization in a general ward, where hypoxemia persisted despite receiving
high concenÂtrations of oxygen. The only comorbidity presented by the patient
was Class I obesity. Upon admission to the ICU, the patient required MVA and
met the criteria for severe ARDS.
During the initial 10 days in the
ICU, the patient underwent four alternating prolonged prone poÂsitioning
cycles, totaling 192 hours in that period and in that position. Until day 23 in
the ICU, the patient received deep sedation and neuromuscular blocking agents.
Complications included infectious events, a sacral pressure ulcer, and
intensive care unit-acquired weakness (ICUAW). After disconÂtinuing
neuromuscular blockade and maintaining a superficial level of sedation, the
patient’s muscle strength, assessed using the MRC scale, scored 38/60. This
score fell below the cutoff point of 48/60. [10].
The patient was weaned from MVA on day 31 of ICU stay, and was discharged from
the hospital on day 52 since admission, without requirÂing supplementary oxygen
and with a MRC score of 50/60. Throughout the hospital stay, the individual had
an average daily intake of 1044 mg of calcium, 728.6 mg of phosphorus, and
737.6 IU of vitamin D. The average daily intake of corticosteroids was 9.29 mg
(0.093 mg/kg/day) of dexamethasone.
Six months after discharge, the
patient preÂsented with pain and limited external rotation movement, and
inability to abduct both hips. A pelvic and hip CT scan was requested,
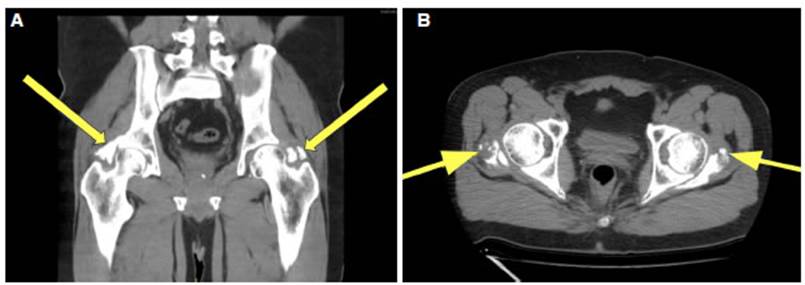
revealing bilateral HO of the hip (Fig. 1A and 1B).
CASE REPORT 2
A 58-year-old patient,
hypertensive and with Class 1 obesity, hospitalized in a general ward and diagÂnosed
with severe COVID-19 pneumonia suffered an ischemic stroke and was transferred
to the ICU. The patient’s respiratory condition deteriorated, requiring MVA.
The patient received two prone positioning cycles, totaling 60 hours within the
first 10 days of ICU stay. He/she experienced infectious complications and a
sacral pressure ulcer. Weaning from MVA was achieved after 39 days. The patient
remained in the ICU for a total of 45 days and was discharged from the hospital
111 days since initial admission. Throughout the hospital stay, he/she had an
average daily intake of 2,359.34 mg of calcium, 1,538.6 mg of phosphorus, and
1,190.8 IU of vitamin D. The average daily intake of corticosteroids was 7.75 mg
(0.072 mg/ kg/day) of dexamethasone. Upon discharge, the paÂtient did not
require oxygen therapy but presented with a moderate right brachio-crural
motor deficit, ataxia, visual field impairment, and gastrostomy tube feeding
due to swallowing disorder. One year post-discharge, there was functional
improveÂment, but with evident limitations in movement unrelated to the motor
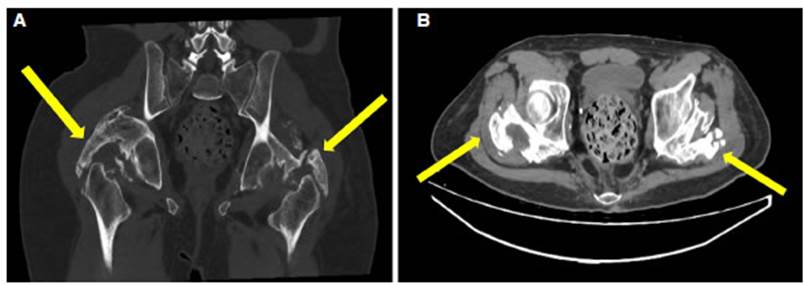
deficit. A pelvic CT scan was performed, revealing heterotopic ossification in
both hips. (Fig 2A and 2B).
As of the current date, there has
been no surgiÂcal opportunity.
DISCUSSION
The published cases of HO in
patients with COVÂID-19 occurred in the context of severe forms of the disease,
involving prolonged hospitalizations and invasive ventilatory
support due to ARDS5-9,11-13. As with any cause of severe
ARDS, paralysis and deep sedation were part of the therapeutic approach.14,15
During the stay of the two
described patients, the occupancy rate of the ICU exceeded between 66 % and
100% its maximum capacity. That is to say, the occupational rate was 16 6% and
200 %, and the workload of the nursing staff, measured by TISS-28, was 72 points,
nearly double the workload manageable by a nurse [own
data]. Infectious complications such as mechanical
ventilation-associated pneumonia, catheter-assoÂciated infections, and pressure
ulcers caused by the decubitus position tripled the average value of the
service. In this context, motor kinesiotherapy was
postponed due to the need to address urgent circumstances, contributing to
prolonged periods of immobilization. The reduced bedside times interfered with
the proper implementation of ventilatory weaning
protocols, resulting in longer periods of MVA and ICU stay. Consequently, there
was greater use of neuromuscular blocking agents and sedatives, generating
prolonged patient imÂmobilization.
Some publications addressing the
pathogenesis of HO consider immobilization as an associated factor, without
specifying the differences between active and passive motion. The work of Stoira et al, shows a four times higher prevalence in
COVID-19 distressed patients compared to those with other causes of ARDS.
We do not know the dose values of
parathyroid hormone, phosphorus, or vitamin D. However, the intake of calcium,
vitamin D, and phosphorus were adequate for baseline needs. Regarding the use
of corticosteroids, the doses were very high, and were consistent with what was
reported by Stoira et al. While some characteristics
specific to SARS-CoV-2 infection are suggested, such as humoral
alterations, disturbances in calcium metabolism, inflammatory response, and
direct muscle injury, the conclusion is that prolonged immobilization is the
only relevant factor in the multivariate analyÂsis. The recommendation is early
passive motion as a preventive method for the development of HO.7
CONCLUSION
Our case report identifies
factors that have been mentioned in the literature as possible causes of HO in
COVID-19 patients. This includes the prolonged use of sedatives and
neuromuscular blockers in patients experiencing intense inflammation. The
critical condition and therapeutic strategy result in long periods of
immobilization during the ICU stay.
However, the above description
does not fully explain the higher prevalence of HO in patients who experienced
ARDS due to COVID-19 when compared to patients who suffered ARDS from other
causes. Thus, there are no differences regarding the inflamÂmatory processes or
the recommendation to use deep analgosedation and
neuromuscular blockade.
We interpret that the workload generated
by patient care during the pandemic peaks had a sigÂnificant influence and
caused unusual situations in daily practice. This included prioritizing respiÂratory
kinesiotherapy over motor intervention, difficulty in
implementing MVA weaning protocols, and less time spent at the patient’s
bedside due to isolation conditions.
As a result, this could have led
to more days of sedatives and neuromuscular blocking agents, prolonged
mechanical ventilation, and the delay or impossibility of passive and active
motion in patients (all circumstances favoring heterotopic ossification).
We believe that the higher
prevalence of HO in severe COVID-19 could serve as a stress marker of the
healthcare system. We think it is relevant to conduct future research to assess
this association.
Conflict of interest
Authors have no conflicts of
interest to declare.
REFERENCES
1. Shreffler J, Huecker
M, Petrey J. The Impact of COVID-19 on Healthcare
Worker Wellness: A Scoping Review. Western Journal of
Emergency Medicine. 2020;21: 1059-66. https://doi.org/10.5811/westjem.2020.7.48684
2. Castro HM, Prieto MA, Muñoz AM. [Prevalence of burnout in healthcare workers during the
COVID-19 pandemic and associated factors. A cross-sectional study]. Medicina. 2022;82:479-86.
3. Sun E, Hanyu-Deutmeyer AA. Heterotopic Ossification. StatPearls. Treasure Island
(FL): StatPearls Publishing; 2022.
4. Shehab D, Elgazzar
AH, Collier BD. Heterotopic ossification. J Nucl Med.
2002;43:346-53.
5. Meyer C, Haustrate M-A, Nisolle
JF, Deltombe T. Heterotopic ossification in COVID-19:
A series of 4 cases. Ann Phys Rehabil
Med. 2020;63:565-7. https://doi.org/10.1016/j.rehab.2020.09.010
6. Meyers C, Lisiecki J, Miller S, Levin A, Fayad L, Ding C, et al. Heterotopic Ossification: A
Comprehensive Review. JBMR Plus. 2019;3: e10172. https://doi.org/10.1002/jbm4.10172
7. Stoira E,
Elzi L, Puligheddu C, Garibaldi
R, Voinea C, Chiesa AF, et al. High prevalence of heterotopic ossification in
critically ill patients with severe COVID-19.Clin Microbiol
Infect. 2021;27:1049-50. https://doi.org/10.1016/j.cmi.2020.12.037
8. Aziz A, Choudhari R, Alexander AJ, Allam E. Heterotopic ossification post COVID-19: Report of
two cases. Radiol Case Rep. 2021;16:404-9.
https://doi.org/10.1016/j.radcr.2020.12.002
9. Vardar S, Ă–zsoy ĂśnĂĽbol
T, Ata E, Yılmaz F. A case report of a patient with
COVID-19 infection and widespread heterotopic ossification. Turk j phys med rehabil.
2022;68:149-53. https://doi.org/10.5606/tftrd.2022.8172
10. Hermans G, Van den Berghe
G. Clinical review: intensive care unit acquired weakness. Critical Care .
2015;19:274. https://doi.org/10.1186/s13054-015-0993-7
11. Serrano ML, Lima Serrano M, González
MĂ©ndez MI, Carrasco Cebollero FM, Lima RodrĂguez JS. Factores de riesgo asociados al desarrollo de Ăşlceras por presiĂłn en
unidades de cuidados intensivos de adultos: revisión sistemática. Med Intensiva. 2017;41:339-46. https://doi.org/10.1016/j.medin.2016.09.003.
12. Van Ochten NA, Shori
A, Puderbaugh MA, Benert J,
Krishnamurthy M. Heterotopic ossification in COVID-19 patient on
anticoagulation with limited treatment options. Medicine: Case Reports and
Study Protocols. 2022. p. e0212. https://doi.org/10.1097/MD9.0000000000000212
13. Brance ML,
Cóccaro NM, Casalongue AN, Durán
A, Brun LR. Extensive progressive heterotopic ossification post-Covid-19 in a man. Bone. 2022;155:116287.
https://doi.org/10.1016/j.bone.2021.116287
14. Chanques G, Constantin
J-M, Devlin JW, Ely EW, Fraser GL, GĂ©linas C, et al. Analgesia
and sedation in patients with ARDS. Intensive Care Med. 2020;46:
2342-56. https://doi.org/10.1007/s00134-020-06307-9
15. Hraiech
S, Yoshida T, Annane D, et al. Myorelaxants
in ARDS patients. Intensive Care Med. 2020;46:2357-72.
https://doi.org/10.1007/s00134-020-06297-8 Â