Autor : SĂvori, MartĂn1-2
1 Pulmonology University Center, Faculty of Medicine. University of Buenos Aires. 2Pulmonology and Tisiology Unit. Hospital Gral. Agudos “Dr.J.M.Ramos MejĂa”. Buenos Aires
https://doi.org/10.56538/ramr.WZQ3579
Correspondencia : MartĂn SĂvori. E-mail: sivorimartin@yahoo.com
Received: 02/18/2023
Accepted: 11/02/2023
The objective measurement of
disability or difficulty in mobilizing due to chronic lung diseases,
particularly Chronic Obstructive Pulmonary Disease (COPD), is a crucial
assessment in the management of patients with this condition.1-3
However, cardiopulmonary exercise testing isn’t widely available
in our country due to the expensive equipment required. Therefore, field
exercise tests represent an attractive alternative. Since Cooper popularized
the first field exercise test (the 12-minute test) in 1968, much research has
been conducted on the topic.4 Today, the
most commonly used field test is the 6-minute walk test, which is a submaximal
test.1-3 Its use and
indication were standardized by the American Thoracic Society (ATS) in 2002 and
more recently in 2014 by several intersocietal
documents of the ATS and the European Respiratory Society (ERS).1-3,5 Other maximal field exercise tests include the
stair climbing test and the shuttle test or “Incremental Shuttle Walking Test”
(ISWT).1-3 The ISWT was
developed by LĂ©ger and Lambert in 1982 for the evaluation of healthy
individuals. The same authors adapted it for athletes between 1984 and 1988,
using a 20-meter circuit.6,7 The test
consisted of 12 steps of progressive intensity.6-7
Singh et al finally adapted it for patients with moderate to
severe COPD thirty years ago, studying 35 patients with two types of protocols:
one with 10 levels and another modiÂfied protocol with 12 levels, each lasting
one minute.8 The initial
speed is 0.5 m/s, increasing by 0.17 m/s until reaching a maximum of 2.37 m/s
on the last level. 8 Two
cones, separated by 9 meters, delimit the circuit with 0.5 meters at each end
for turning. In summary, a simple audible signal tells the patient that they
should be at one end, and a triple signal every completed minute indicates an
increase in walking speed. In the first minute or level, the patient completes
the circuit three times (3 x 10 m = 30 meters); in the second level, four times
(4 x 10 m = 40 meters), and so on. The test is considered complete when the
patient informs that they cannot maintain the walking pace for two consecutive
sections, being more than 0.5 meters away from the cone, not completing two
consecutive sections being more than one meter away from the cone.1-2
WHY IS IT SO USEFUL?
The operational characteristics
(reproducibility and correlation with other physiological paramÂeters) make it
ideal for multiple indications (Table 1). It shows good correlation with the
6-minute walk test (r=0.68), but, more importantly for its everyday clinical
application, it has moderate to high correlation with the patient’s aerobic
capacÂity (peak oxygen uptake [VO2p])
(r=0.68-0.88).8-12 Singh et al
studied the correlation between the ISWT and VO2p in 19 patients with different deÂgrees
of COPD (FEV1 [forced
expiratory volume in the first second] of 0.5 to 3.1 L), also observing a high
correlation between the two tests (r=0.88).11
Elias Hernandez et al correlated the ISWT with the VO2 determined in
a maximal test with a cycle ergometer, resulting in a slightly lower
correlation (VO2 in L/min of
r=0.71 and VO2 in ml/kg/min
of r=0.68).12 In our group
of 21 patients with severe obstruction, the correlation was high (R2 = 0.8135,
p<0.001).13 In places
where cardiopulmonary tests are not available to assess aerobic capacity,
either due to a lack of equipment or high costs, applying the prediction
formula basing on the maximum distance walked in the ISWT can predict the paÂtient’s
VO2p
with high accuracy. The formula we developed is:
VO2 peak
mL/kg/min =
0.0438 x ISWT meters + 0.8569.13
For distances above 300 meters walked
in the ISWT, a VO2 peak greater
than 13 mL/kg/min was always observed. This could be used as a parameter for
predicting success in lung resection surgeries of patients with uncertain
predictions based on FEV1 (at
the functional resectability limit) and limited
access to a cardiopulmonary test for measuring the VO2
peak.14
Another important characteristic
is its simplicÂity in terms of the resources required and the speed at which results
can be obtained: it only requires an audio signal, a 10-meter hallway, an oximeter, and a chart for evaluating dyspnea/muscular faÂtigue
on the Borg scale. In addition to heart rate, the variables measured include
blood pressure at the beginning and end, and the distance walked when
completing the last section before the study is considered complete. The
criteria for ending the test were highly variable until standardized by the
ATS/ERS, as defined above.1-2.
There is also a medical criterion, according to which the test may be stopped
if oxygen saturation is less than 80 %.1-2
However, the recommendation does not specify other situations
such as angina, loss of stability, altered consciousness, or intermittent
claudication, which should also be considered as reasons for stopping the test
according to the opinion of this author.1-2
The reproducibility of the test is very good, and two studies
should be conducted, separated by 20 to 30 minutes, with the one covering the
greater distance being considered for evaluation.1-2
The ISWT predicts the risk of
hospitalizations and even mortality in COPD.1-3
ElĂas Hernández et al demonstrated high
correlation between the meters walked, dyspnea, and heart rate in patients with
severe COPD, with high reproducibility.12
We did not find a significant correlation between the ISWT and
different spirometric indices, although there was a
trend showing that more meters walked = lower degrees of bronchial obstruction.13 No
significant correlation was observed, either, in the quality of life scale used
for chronic respiratory diseases, similar to other authors.11,13 However, ElĂas
Hernández et al found a significant moderate correlation between the ISWT and
parameters of lung function and dyspnea, but not with quality of life.12
It has been suggested that the
clinically sigÂnificant minimum difference was 4 sections or 40 meters, and
more recently, 35-36 meters.15-16 Our group has
investigated the response of the ISWT to different non-pharmacological intervenÂtions
(respiratory rehabilitation and non-invasive ventilation).17-18
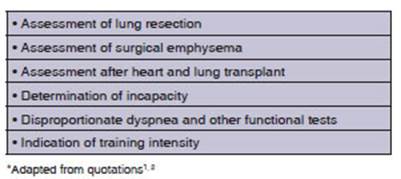
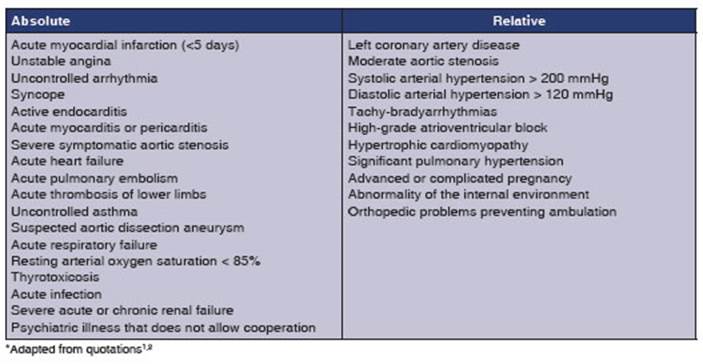
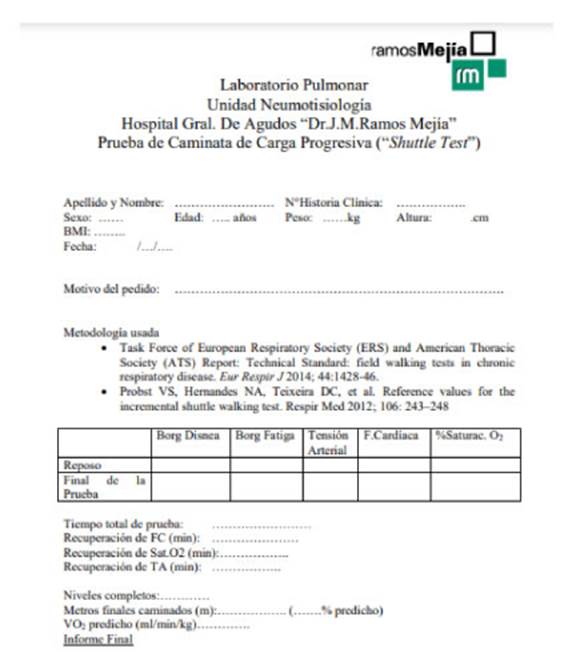
Table 1 highlights its
indications, and Table 2 outlines its contraindications. Figure 1 shows a
report model from our Hospital Ramos MejĂa in CABA.
Revill et al have introduced a variant of the ISWT, known as the Endurance
Shuttle Walk Test, as an assessment of exercise
endurance capacity (a submaximal test at 75 to 95 % of the initial ISWT maximum
speed), comparing it with a treadmill.19 They evaluated 10 patients
with severe COPD and found no differences in heart rate and dyspnea responses
between both tests.19 This type of test should be carried out only once.2
It is a highly reproducible test, very sensitive to changes with therapeutic
interventions. Jolly et al assessed COPD patients after an outpatient
respiratory rehabilitation program (hospital-based vs
home-based), and found greater sensitivity to post-training changes.17
MartĂnez Fraga el al also
determined significant changes in COPD patients receiving non-invasive ventilatory assistance with pressure support during
exercise.18
WHY ISN’T IT USED?
With regard to the
ISWT, one of the main reasons why the test is not widely used is the lack of
trainÂing among physicians. Physicians are the ones who should perform this
field test, given that it is a maximal exercise test for legal reasons, and
therefore may lead to acute cardiovascular or cerebrovascular events, but this
is not clarified in the latest regulations.1-3 Another reason is
that the test isn’t widely disseminated. It should be proposed on a local and intersocietal level with cardiologists and thoracic
surgeons, including loÂcal dissemination guides, as it happened with the
six-minute walk test.20-21
As for the test
itself, the circuit is very short for patients who are not functionally
incapacitated, and the turn in the same direction can cause dizÂziness, as
minutes pass by. It is essential to always insist on providing adequate
training and informaÂtion before the patient’s study, as many patients find it
difficult to understand the test’s methodÂology regarding the synchronicity of
the pace in reaching each end of the circuit and the different meanings of the
audio. In the past, the provision of audio signals was one of the main limiting
factors, but nowadays, through the Internet and various applications, it is
easier.
Another issue with
the test is that it narrowly evaluates physiological variables of exercise and
its changes, and it does not evaluate its metabolic response. Therefore, unlike
the cardiopulmonary test with expired gas measureÂment, it does not allow the
differentiation of concomitant diseases and their relationship with exercise
intolerance.
Another problem is
the safety of the test, in the opinion of the author, which is not adequately
declared in international regulations. It is stated that “it shows rare
complications, and no adverse events have been reported in clinical studies”.2
I suggest doing it with cardiac telemetry to have readings of cardiac
electrophysiological changes as the test progresses, as it is a maximal test as
would be done in any cardiac ergometry or maximal carÂdiopulmonary
test. Certainly, since it is not propÂerly standardized in the international
guideline, if telemetry is not available, it is possible to request prior
cardiovascular risk assessment to rule out the occurrence of arrhythmias or
unknown coronary artery disease.
Another area that needs
to be developed is the investigation of the minimum clinically important
difference (MCID), which should be explored in other diseases apart from COPD.22-29
The ISWT has been studied to assess patients with advanced cancer, pacemakers,
chronic heart failure, asthma, cystic fibrosis in adults, interstitial lung
diseases, and even in the pediatric population.22-29 In cardiac
patients, this test would be of great value due to its close estimate of the
predicted VO2 max in the context of pre-cardiac transplant
evaluation, especially in areas where cardiopulmonary tests aren’t easily
available.
Another issue is the
limited number of tables with normal predictive values. Besides the small
number, there is the restricted age range and enrolled ethnicity. There are
four tables of Latin subjects (three from Brazil) and one from the United
Kingdom.30-34 And there are two pediatric tables.30-31 In
adults, Probst et al estimated preÂdictive values in
242 subjects between 30 and 60 years from Southern Brazil.32 The determining
factors affecting the prediction of normality are age, gender, and body mass
index (BMI), which explain 71 % of the prediction.32 The other table
from Brazil is from the state of SĂŁo Paulo, which establishes reference values
in 131 subjects beÂtween 40 and 84 years .33 The determining factors
were age, gender, height, and weight, explaining 50.3 % of the prediction.33
From the group of Singh in Leicester, United Kingdom, reference values have
been determined in 114 subjects aged 40 to 90 years.34 Age, FEV1,
BMI, maximum voluntary contraction of the quadriceps, and a physical activÂity scale explain 50.4 % of the prediction.34 This author
suggests that, until we have more studies with tables of normal values, we
should use the predictive table of Probst et al for
adults under 40 years, both the Probst et al and the JĂĽrgensen et al tables for individuals between 40 and 60
years, and also the Probst et al and JĂĽrgensen et al tables for subjects above 60 years, as the
subjects in these tables are probably closer to the ethnic mix of our country.32-33
Regarding the endurance shuttle
walk test, it is only used in clinical studies because it is very
time-consuming as it requires a prior incremental test, and it is validated in
patients with COPD and has very high sensitivity to therapeutic inÂtervention
responses.19 The MCID for this test has been established at 65 to 85
seconds after bronchodilation and 180 seconds
post-respiratory rehabilitation.2
THE FUTURE OF ISWT
The ISWT is a maximal field exercise
test: simple, standardized, and potentially more available in our country than
the oxygen consumption test. It allows for the high-reliability assessment of
the aerobic capacity of patients with COPD. Further research should be
conducted in other diseases. Despite the fact that it has been developed speÂcifically
for COPD patients thirty years ago, its daily clinical use is still limited.
Areas of research should include having predictive value tables more
representative of our population, validatÂing it in other chronic respiratory
diseases, and thoroughly studying the safety of the test. In the meantime, it
is necessary to disseminate its utility through related Medical Societies,
generÂating documents and dissemination and training activities for the medical
community. In a country with limited availability of equipment and high costs
of cardiopulmonary tests (oxygen consumpÂtion), the ISWT is an ideal tool for
evaluating the functional capacity of patients with COPD and other diseases.
Conflict of interest
The author declares having no
conflict of interest regarding the writing of this manuscript.
Acknowledgement
The author thanks Dr. Javier Brea
Folco for his incentive to write this critical
review.
REFERENCES
1. Holland AE, Spruit M, Troosters T, et al. An
official European Respiratory Society and American Thoracic Society technical
standard: field walking tests in chronic respiraÂtory disease. Eur Respir J. 2014;44:1428-46. https://doi.org/10.1183/09031936.00150314
2. Singh S, Puhan M, Andrianopulos V, et al.
An official systematic review of the European Respiratory Society and American
Thoracic Society: measurement properties of field walking tests in chronic
respiratoÂry disease. EurRespir J. 2014;44:1447-78.
https://doi.org/10.1183/09031936.00150414
3. Puente-Maestu L, Palange
P, Casaburi R, et al. Use of exercise testing in the evaluation of
interventional efficacy: and official ERS Statement. Eur
Respir J. 2016;47:429-60.
https://doi.org/10.1183/13993003.00745-2015
4. Cooper R. A means of assessing maximal oxygen intake. JAMA.
1968;203:201-4.
https://doi.org/10.1001/jama.1968.03140030033008
5. American Thoracic
Society. ATS Statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111-7. https://doi.org/10.1164/ajrccm.166.1.at1102
6. LĂ©ger L, Lambert
K. A maximal multistage 20-m shuttle run test to predict VO2 max. Eur J Appl Physiol. 1982;49:1- 12. https://doi.org/10.1007/BF00428958
7. LĂ©ger LA, Mercier
D, Gadoury C, Lambert J. The multi-stage 20 metre shuttle run test for aerobic fitness. J Sports Sci.
1988;6:83-91.
https://doi.org/10.1080/02640418808729800
8. Singh S, Morgan M,
Scott S, Walters D, Hardman A. DeÂvelopment of a shuttle walking test of
disability in patients with chronic airways obstruction. Thorax 1992;47:1019-24. https://doi.org/10.1136/thx.47.12.1019
9. Puente
Maestu L. Physiological rationale of commonly used
clinical exercise tests. Pulmonology. 2020;26:159-65.
https://doi.org/10.1016/j.pulmoe.2019.10.004
10. Parreira VF, Janudis-Ferreira T, evans RA, Mathur S, Goldstein RS,
Brooks D. Measurement properties of the Incremental Shuttle Walk Test: a
systematic review. Chest. 2014;145:1357-69.
https://doi.org/10.1378/chest.13-2071
11. Singh S, Morgan
M, Scott S, et al. Comparison of oxygen uptake during a conventional treadmill
test and the shuttle walking test in chronic airflow limitation. Eur Respir J. 1994;7:2016-20.
https://doi.org/10.1183/09031936.94.07112016298
12.
ElĂas Hernández M, Ortega Ruiz F, Fernández Guerra J, Toral MarĂn H, Sánchez
Riera H, Montemayor Rubio T. ComparaciĂłn de un test de paseo de carga
progresiva (shuttle walking
test) con una prueba de esfuerzo en cicloergĂłmetro en
pacientes con EPOC. Arch BroncoÂneumol.
1997;33:498-502. https://doi.org/10.1016/S0300-2896(15)30531-7
13.
SĂvori M, Sáenz C. Prueba de caminata de carga
progresiva (shuttle test) en la Enfermedad Pulmonar
Obstructiva CrĂłnica. Medicina Buenos Aires. 2010;70:305-10.
14. Olsen GN. The
evolving role of exercise testing prior to lung resection. Chest. 1989;95:218-25.
https://doi.org/10.1378/chest.95.1.218
15. Singh S, Jones P, Evans R,
Morgan M. Minimum clinically important improvement for the Incremental Shuttle
WalkÂing Test. Thorax. 2008;63-775-7.
https://doi.org/10.1136/thx.2007.081208
16. Evans RA, Singh SJ. Minimum
important difference of the incremental shuttle walk test distance in patients
with COPD. Thorax. 2019;74:994-5.
https://doi.org/10.1136/thoraxjnl-2018-212725
17.
Jolly E, Sivori M,
Villarreal S, Almeida M, Saenz C. EnÂfermedad
Pulmonar Obstructiva CrĂłnica: Entrenamiento domiciliario versus ambulatorio
hospitalario. Medicina Buenos Aires. 2014;74:293-300.
18.
MartĂnez Fraga A, SĂvori M, Delgadillo S., et al. La
venÂtilaciĂłn no invasiva mejora los resultados en las pruebas de ejercicio en
pacientes con EPOC. Rev Am Med Respir.
2011;3:125-33.
19. Revill
S, Morgan M, Singh S, Willimas J, Hardman E. The
endurance shuttle walk: a new field test for the assessment of endurance
capacity in chronic obstructive pulmonary disease. Thorax. 1999; 54:213-22.
https://doi.org/10.1136/thx.54.3.213
20.
Dávolos I, Brea Folco JC, Bucay C, et al. Prueba de Marcha de 6 minutos: 1ra. parte. Historia, Indicaciones y evidenÂcia. Situaciones
especiales. Documento Intersocietario de la Sociedad
Argentina de CardiologĂa y la AsociaciĂłn Argentina de Medicina Respiratoria. Rev Am Med Respir. 2022;22:1-20.
21. Brea Folco
JC; Dávolos I, Arce S, et
al. Prueba
de Marcha de 6 minutos: 2da.parte. Aspectos técnicos. Estandarización.
Documento Intersocietario de la Sociedad Argentina de
CardiologĂa y la AsociaciĂłn Argentina de Medicina RespiÂratoria. Rev Am Med Respir. 2022;22:21-33.
22. Booth S, Adams L. The shuttle
walking test: a reproducible method for evaluating the impact of shortness of
breath on functional capacity in patients with advanced cancer. Thorax. 2001; 56:146-50.
https://doi.org/10.1136/thorax.56.2.146
23. Garrod
R, Mikelsons C, Paul E, Wedzicha J. Randomized controlled trial of
domiciliary noninvasive positive presÂsure ventilation and physical training in
severe COPD. Am J Crit Care Respir Med. 2000; 162:1335-41.
https://doi.org/10.1164/ajrccm.162.4.9912029
24. Payne G, Shekan
J. Shuttle walking test: a new approach for evaluating patients with
pacemakers. Heart. 1995;75:414-8.
https://doi.org/10.1136/hrt.75.4.414
25. Kell
SS, Chambers J, Francis D, et al. Shuttle-walk test to assess chronic heart
failure. Lancet. 1998;352:705.
https://doi.org/10.1016/S0140-6736(05)60821-5
26.
Morales F, MartĂnez A, MĂ©ndez M, et al. A shuttle walk test for assessment of functional capacity in chronic
heart failure. Am Heart J. 1999;138:291-8.
https://doi.org/10.1016/S0002-8703(99)70114-6
27. Bradley J, Howard J, Wallace
E, Elborn S. Validity of a modified shuttle test in
adult cystic fibrosis. Thorax. 1999; 54:437-9.
https://doi.org/10.1136/thx.54.5.437
28.
Goncalves Labadessa I, Borghi-Silva A, Sánchez GarcĂa de Araujo A, Galhardo Rizatti FP, Di Lorenzo
VA. Reliability of
cardiorespiratory and metabolic responses during incremental shuttle test in
adult subjects with asthma. Respir Care. 2019;64:55-62.
https://doi.org/10.4187/respcare.06112
29. Singh S, Moiz
JA, Ali MS, Talwar D. Reliability, validÂity and
responsiveness of the incremental shuttle walk test in patients with
interstitial lung disease. J Cardiopulm Reh. Prev 2018;38:425-9.
https://doi.org/10.1097/HCR.0000000000000327
30.
De CĂłrdoba Lanza F, Do Prado Zagatto E, Cunha Slva J, et al. Reference equation for the incremental shuttle walk test in children and
adolescents. J
Ped. 2015;167:1057-61. https://doi.org/10.1016/j.jpeds.2015.07.068
31.
Ciudad D, DĂaz P, Orellanda J, Soto C. Prueba de
caminata de carga progresiva (incremental shuttle walking test) en niños sanos. Rev
Chil Enf Respir. 2018;34:160-4.
https://doi.org/10.4067/s0717-73482018000300160
32.
Probst V, Hernandes N,
Teixeira DC, et al. Reference values for the
incremental shuttle walking test. Respir Med
2012;106:243-8.
https://doi.org/10.1016/j.rmed.2011.07.023
33.
JĂĽrgensen SP, De Oliveira Antunes
CL, Tanni SE, et al. The incremental shuttle walk test in older brazilÂian adults. Respiration.
2011;81:223-28. https://doi.org/10.1159/000319037
34. Harrison SL, Greening NJ, Houchen L, et al. Reference values for the incremental
shuttle walking test in a healthy population. Thorax.
2011;66 (Suppl 4):A55-A56.
https://doi.org/10.1136/thoraxjnl-2011-201054b.120